What new waves of a pandemic might look like
Health / / December 29, 2020

Popular science edition about what's happening in science, engineering and technology right now.
During the First World War, the Chinese were, to put it mildly, not up to the rest of the world: the country was fighting for power, the Chinese either declared war on Germany, then recognized this decision as unconstitutional, then declared again. When the allies demanded help from them, the Chinese began to equip a kind of "construction battalion" for Europe. Chinese workers had to dig trenches, lay out telegraph wires, build barricades and railways.

In 1918, the country beganPaths of Infection: The First World War and the Origins of the 1918 Influenza Pandemic an epidemic of "winter sickness" (today we would call it a "cold") - so it is not surprising that people with influenza were also among the units of the Chinese labor corps, which were sent to war.
The result is known to us: bullets and artillery were killed in four years of war
World War I. Killed, wounded, and missing about 8.5 million soldiers, nearly 13 million civilians were victims of starvation and murder. The number of victims of "Spanish flu" taken out of China by unarmed workers reaches 50 million in two years of the pandemicUpdating the Accounts: Global Mortality of the 1918-1920 "Spanish" Influenza Pandemic.In 2016, Canadian historians reconstructedReviewing the History of Pandemic Influenza: Understanding Patterns of Emergence and Transmission the circumstances of the global pandemic. Although the picture was slightly different from country to country, there are three distinct waves of the pandemic around the world, occurring in the spring of 1918, the fall of 1918 and the winter of 1918-1919. Most of the victims of the pandemic died in the second wave.

Most of the Chinese went to Europe through Canada - they were dropped off at the port, put on trains, and then taken to the other side of the country and transported to New York. From there they were sent to Scotland and then to France, where they finally found themselves in a war zone.
The Canadian Prime Minister quite reasonably feared that the Chinese workers would scatter on the way. To prevent this from happening, he assigned soldiers to the carriages. Here, the first outbreak in 1918 happened: the Canadians blocked the route for the next Chinese units, but the disease had already burst out - the soldiers guarding the Chinese began to get sick.
One of the first "international hubs" of the disease was the British port city of Plymouth, a place where Chinese workers also traveled. From this port, along with the infected sailors, the Spaniard arrived in Europe, Africa, New Zealand and the United States. In four months, the disease spread to half the globe and began to kill.

The wave subsided in January 1919 - after most of the people on the planet had been ill. Susceptible to virus people can be compared to "fuel": as soon as most of the fuel "burned out", the "machine" of the epidemic stalled. Therefore, the third wave was already more like a small flash. In the winter of 1918-1919, people without immunity to the Spanish flu became infected from time to time, but there were already few of them, so the third wave turned out to be much smaller than the second.
In 1918, there was a shortage of medical personnel in the rearReviewing the History of Pandemic Influenza: Understanding Patterns of Emergence and Transmission: doctors and nurses were at war. Hospital places quickly ran out, so schools and other public places began to be adapted for hospitals. But even those doctors who stayed at home could do little to help the sick - vaccines and medicines for influenza had not yet been invented. Ordinary people were savedGreat Pandemic: The United States in 1918-1919 home remedies like a mixture of water, salt and kerosene. The demand for alcohol has sharply increased - many hoped for alcohol (even some doctors recommended drinking it to protect against the flu).
They didn't really know how to diagnose the flu. All the doctors knew was that the disease spreads with sneezing and cough. Because of this, influenza was often confused with other diseases and was not properly recorded - so that outbreaks of the disease were often passed by the documents. As a result, measures that could contain the spread of the disease were applied unevenly1918 Pandemic (H1N1 virus) - either too late, when the optimal time to contain the disease has already been missed.
Influenza-1918 and coronavirus-2019
The American Center for Infectious Disease Research and Policy (CIDRAP) believes that the best modelCOVID-19: The CIDRAP Viewpoint to understand the coronavirus disease pandemic, it is pandemic influenza and not previous outbreaks of coronavirus diseases.
The coronavirus disease COVID-19 associated with SARS-CoV-2 is not very similar to its other coronavirus predecessors. The SARS ‑ CoV ‑ 1 SARS epidemic of 2003 was quickly stopped, so that by 2004 there were noSevere acute respiratory syndrome (SARS) a new case, and MERS-CoV, in principle, could notMiddle East Respiratory Syndrome (MERS) cause an international pandemic.
According to the researchers, the similarities between past influenza pandemics and the coronavirus disease pandemic are striking in several ways:
- Population susceptibility. Both the SARS ‑ CoV ‑ 2 coronavirus and the influenza A (H1N1) virus are completely new viral pathogens that humanity does not have immunity. This means that anyone who encounters each of these viruses is at risk of getting sick.
- "Lifestyle" and distribution method. Both viruses settle in the respiratory tract and are transmitted along with the smallest droplets of saliva.
- Transmission by asymptomatic patients. Both viruses can be spread by people who don't even know they are sick.
- Epidemic potential. Practice shows that both viruses are capable of infecting many people and quickly spreading around the world.
But there are also differences. COVID-19 is more infectious than influenza: reproduction index (R0)Unraveling R0: Considerations for Public Health Applications higher for coronavirus infection. It has a longer incubation period (five days versus two), and a higher percentage of asymptomatic carriers (up to 25 percent versus 16 in flu). Moreover, the time of greatest contagion, most likely, falls on the asymptomatic stage - in contrast to the flu, for which this moment occurs in the first two days after the onset of symptoms. Therefore, if influenza R0 within 1.4-1.6Modeling influenza epidemics and pandemics: insights into the future of swine flu (H1N1), then the coronavirus, according to various estimates, has R0 maybe from 2.6Report 9: Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand up to 5.7High Contagiousness and Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2.
So the Spanish flu pandemic of 1918-1920 and COVID-2019 can be comparedReport 9: Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand - and the comparison will be "in favor" of the coronavirus disease. Considering that at the peak of the Spanish flu, one patient infectedEstimates of the reproduction number for seasonal, pandemic, and zoonotic influenza: a systematic review of the literature two, then the hypothetical "tsunami" COVID-2019 could be about one and a half to three times more dangerous.
Will there be a second wave
Outbreak of any infectious disease stopswhen its effective reproductive number, Re, becomes less than one. This happens at a time when the number of people vulnerable to the virus decreases, so that the sick person can no longer infect anyone else.
To calculate how many people must become immune for the pandemic to stop, one must take into account the proportion of people (s) susceptible to infection. To stop the epidemic, sR0 < 1. That is, s <1 / R0. And if R0 coronavirus infection - 2.6-5.7, then that Re in a specific case, it has become less than one, the proportion of people susceptible to infection should be less than 40–20 percent.
This can be achieved in the following ways:
- If 60-80% of the population falls ill.
- If the same 60-80% of people succeed vaccinate.
- If all infectious people are isolated from vulnerable people and their contacts controlled.
In this situation, the pandemic will stop and there will be no second wave. True, this will work only if the immunity of those who have been ill or vaccinated is stable.A Perspective on Multiple Waves of Influenza Pandemics - otherwise, after some time, people begin to become infected in the second circle. However, researchers do not yet know exactly how strong the immunity to SARS ‑ CoV ‑ 2 will be. It must be borne in mind that, in principle, it is not formed for coronavirus infectionsCoronavirus infections and immune responses strong immunity, so that the risk of re-infection with another strain of coronavirus cannotOn the origin and continuing evolution of SARS-CoV-2 discounted.
As in the days of the Spanish flu, humanity still has no protection against coronavirus disease. There are no effective drugs - and they are unlikely to appear in the near future - and we will be able to count on the appearance of a vaccine only in a year or two. However, we also cannot do nothing with the disease based on herd immunity, because then the coronavirus will kill 0.9-7.2%Coronavirus disease 2019 (COVID-19): Epidemiology, virology, clinical features, diagnosis, and prevention sick, so the cost of immunity will be too high.
All that remains for humanity is to implement containment measuresThe effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modeling study diseases: either declare quarantine (as in China, Italy, Denmark and England), or urge the population to social distancing (approximately as in some US states and in Russia). These measures can reduce the number of new infections and save thousands of lives - but they will not help to acquire an immune shield.
If we give up social distancing prematurely, Re will remain the same as it was. And since it is very difficult to understand when it is already possible to start abandoning measures to contain the disease, we have to admit that the chance of a second wave of COVID-19 is very high.Beware of the second wave of COVID-19.
Lesson from St. Louis
There is little information about how they tried to contain the flu in Europe during the Spanish flu - almost no documents about this have been preserved due to the war. The war did not affect the territory of the United States, so there are more records in this country. Therefore, we know that in American cities and at military bases, where they managed to implement containment measures (quarantine, school closings, banning public gatherings), mortality was lowerNonpharmaceutical Influenza Mitigation Strategies, US Communities, 1918-1920 Pandemic, and the peak of the epidemic came later. True, in many communities, local government guidance on the dangers of influenza was poorly understood.Great Pandemic: The United States in 1918-1919, and often ignored altogether.
For example, the Spanish flu arrived in St. Louis in October 1918. With the support of the Mayor, Health Commissioner, Dr. Max Starkloff, closed city schools, theaters, cinemas, places of entertainment, forbidden to use the tram and gather in a company of over twenty man. He even closed churches for the first time in the city's history. The archbishop was very unhappy, but could not reverse the doctor's decision.

In addition to what today would be called "social distancing", Dr. Starkloff has worked with the public: distributed among the townspeople a brochure in which he urged to cover your mouth with your hand when coughing so as not to spread disease. The brochure was printed in eight languages - there was even a version in Russian and Hungarian.
Thanks to his efforts, the effective reproductive number (Re) became less than one. However the St. Louis are too earlyHow some cities ‘flattened the curve’ during the 1918 flu pandemic relaxed. In the eleventh week of social distancing, the government decided the danger was over and lifted the restrictions. People again threw themselves into schools and churches, and again they re-infected each other. As a result, Re grew again - and the second wave of the disease began, more powerful than the first. Two weeks later, the government caught on and resumed restrictive measures, the epidemic began to decline, but the dead, of course, could not be returned.

After the end of the pandemic, it became clear that even these "half-hearted" measures were beneficial. In St. Louis, 1,703 people died - half the number of neighboring Philadelphia. True, restrictive measures were also introduced in the city - but after the parade for 200,000 people was held.
What waves can be
In the twenties of the XX century, people knew very little about the nature of the Spanish flu - there was not even an exact certainty that it was viruses, and not bacteria, that caused it.Reviewing the History of Pandemic Influenza: Understanding Patterns of Emergence and Transmission. Since then, mankind has accumulated knowledge and survived three more similar pandemics - and none of them was as destructive as the 1918-1920 pandemic.
We have not learned to treat viral respiratory diseases, but we have learned to contain them. The effectiveness of deterrent measures can also vary - therefore, CIDRAP experts suggestCOVID-19: The CIDRAP Viewpoint at least three scenarios, according to which the “second wave” could theoretically go.
"Surf"

How it might look. Following the first wave, the same waves will come once every 1-2 years, and starting from 2021 - slightly smaller waves.
Under what conditions? If everything continues to go the way it goes. Eventually, states will have to loosen their deterrent measures, and people will have to to go to work. Despite social distancing, over time, people begin to become infected again. When the pandemic reaches a certain threshold, the restrictions will have to be reintroduced and the new pandemic will subside. Small waves will “roll over” humanity until 60-70% of people get sick - or until a vaccine appears.
"Tsunami"

How it might look. In the fall (or winter) of 2020, a "tsunami" will hit humanity, followed by several smaller waves in 2021 - as in the case of the Spanish flu.
Under what conditions? If the first wave of humanity does not teach anything. Instead of preparing for the second wave, the government will ignore the "warning" and will not spend money on staffing hospitals, and citizens will live as before: go to concerts, restaurants and other places of congestion people. The situation will be similar to the "surf", only the next wave will immediately be gigantic - and will quickly gain height. In this situation, 60–70% of those who have been ill, necessary for herd immunity, will be recruited quickly - but with great losses.
"Ripple"
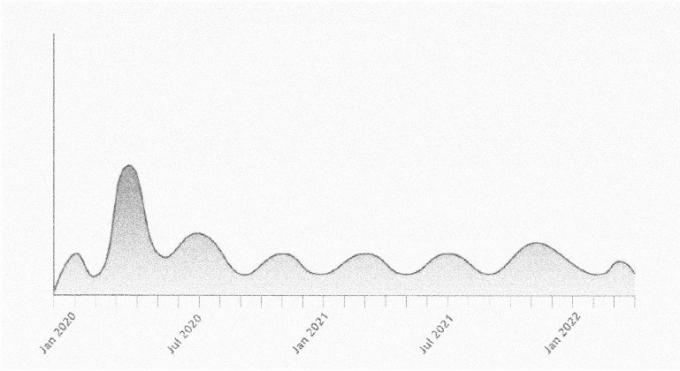
How it might look. Like surf - but without having to re-introduce restrictive measures. That is, there will be no new pandemics, but in 2020-2021 there will be several minor epidemics.
Under what conditions? If the SARS ‑ CoV ‑ 2 coronavirus quickly adapts to its new human hosts and therefore loses its lethal potential. This has not yet happened with influenza pandemics. But it is possible that it will be different with the coronavirus. SARS ‑ CoV ‑ 1 disappeared after the first epidemic - but it was much less contagious. In general, viruses of this family (for exampleProjecting the transmission dynamics of SARS-CoV-2 through the postpandemic period, the less dangerous HCoV ‑ OC43 and HCoV ‑ HKU1) tend to circulate constantly in the population and wait for the right moment to provoke another epidemic.
Read also🧐
- How will the coronavirus pandemic develop and how will it end
- 13 films that predicted the coronavirus pandemic and more
- "The soldier's wife told ...": where do the rumors and fakes about the pandemic come from and why people spread them